Preclinical in vivo molecular imaging is widely regarded as a key tool within the drug discovery and development pipeline, giving researchers clear visibility of cellular changes at a molecular level. Techniques – or modalities – such as optical, PET and SPECT imaging provide high specificity and wide applicability, as well as the ability to monitor several molecular events and identify key molecular markers. The result is a deeper understanding of disease progression, and the mode of action and pharmacokinetics of potential therapeutics.
If we consider small animal optical imaging systems specifically, these now enable researchers to combine a number of imaging modalities using the same instrument, thereby paving the way for a better understanding of physiological and disease mechanisms in the preclinical setting. For example, one such system provides five imaging modalities as standard, allowing for co-registration of molecular events with access to bioluminescence, multispectral VIS-NIR fluorescence, unique direct radioisotopic imaging, and Cerenkov radiation. A high speed digital X-ray scanner adds to the functional images with morphological features.
Q: Can you give us your perspective on how far we have come with optical imaging for preclinical research?
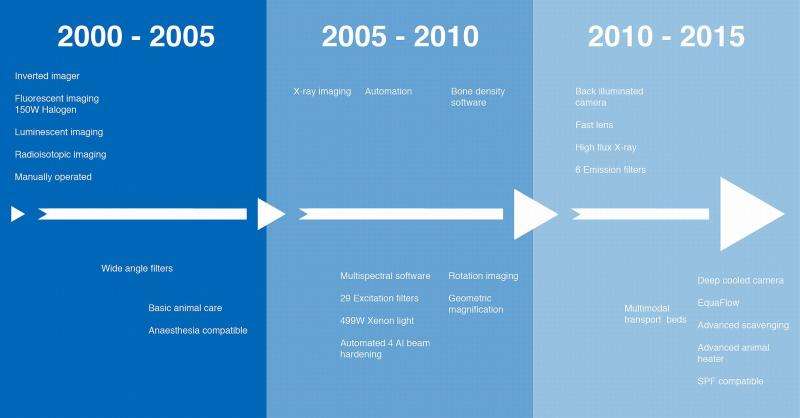
“If we look back to the early 2000s, this was the time that commercial multimodal small animal imaging systems were becoming affordable for the research community in pharma. Even at this early stage, systems typically featured a combination of luminescent, fluorescent and/or radioisotopic imaging. In addition, X-ray functionality was added to provide a precise anatomical reference onto which molecular data could be overlaid.
“Automation was later introduced into optical imaging systems, bringing efficiencies to the lab and allowing throughput to increase. Significant software development improved ease of use and accessibility of data. More recently, advances in system technologies have enabled features such as geometrical magnification and back-illumination to improve resolution and sensitivity for multimodal X-ray and optical imaging. Cell tracking, monitoring inflammation and other physiological changes as well as using molecular probes to assess disease development have all been enabled by these systems developments.”
Q: For our readers who are new to the field, can you give us an overview of the modalities that are commonly used – I assume bioluminescence and fluorescence are two that are key?
“Yes, that’s right. Bioluminescence (BLI) is most commonly used to monitor tumour cells, infections, gene expression and monitoring response to therapy in real-time. It works by the detection of luciferase light emission from engineered cells and can also be quantified and used as a reference for disease progression. Low-cost and non-invasive, this technique is ideally suited to preclinical, longitudinal animal studies.”
“On the other hand, fluorescence (FLI) is used for imaging of specific biological processes, molecular events and tissue vascularity. Exogenous probes labelled with fluorophores target cell specific markers and the light emission from the fluorophore after excitation is detected and quantified. Nowadays, it is more common to use near-infrared (NIR) proteins or probes as they emit stronger signals than the more traditional colours of red and green.
“Although not so widely used, direct radioisotopic imaging (DRI) is a proven, additional method in obtaining a full understanding of disease progression. Here, radioisotopes injected into a model emit gamma rays that are detected throughout the tissues and bones. An increased uptake of a radioisotope - and hence increased gamma emission - in a specific location indicates increased activity such as tumour growth.”
“Cherenkov Imaging (CLI) has only recently been applied in preclinical imaging to monitor therapeutic efficacy. CLI uses light emission from commonly used medical isotopes. Cherenkov radiation is produced when charged particles travel faster than the speed of light within the tissues, allowing the detection of light emitted from the radioactive isotopes.
“Finally, X-ray is most usefully employed in preclinical research to give anatomical reference for molecular imaging. When analyses are undertaken within the same multimodal system, all the resulting images can be accurately layered using intelligent software to ensure precise automatic co-registration of images, thereby providing researchers with a better understanding of the molecular mechanism or interaction of interest, with a precise anatomical reference.”
Q: Tell us about the latest developments – and what new opportunities these open up for researchers?
“Technological advances are increasingly aiding researchers to optimize in vivo testing in the preclinical setting and translate their work from in vivo models into the clinical situation. Instrument manufacturers are working to provide them with easy to use, time saving research tools that will enable higher test throughput and enhance their insight through facilitating more accurate analyses and improved access to useful data.
“In preclinical imaging, for example, the development of multimodal systems is set to transform research practice, facilitating use of complementary imaging techniques to improve understanding of disease progression and drug efficacy. One such multimodal imaging system* enables all five imaging modalities outlined above to be conducted consecutively, allowing for co-registration of molecular events with access to bioluminescence, multispectral VIS-NIR fluorescence, unique direct radioisotopic imaging and Cerenkov radiation. A high speed digital X-ray scanner with industry-leading resolution and reflectance modes enhance the optical functional images with morphological features.
“Similarly, technological advances have also emerged to tackle the issues of detection limits often faced by researchers. Enhanced camera capabilities now bring a new level of sensitivity, speed and versatility to non-invasive procedures, enabling researchers to discover important biological mechanisms in disease to inform treatment and monitoring. By cooling the camera to less than -90° C and using exceptionally low read noise electronics, unprecedented performance levels during extremely low-light applications - such as bioluminescence and Cerenkov imaging - are achieved.
“Cross platform functionality – in both software and hardware - is an area where we have seen some of the most interesting developments over the past decade, and where we predict further innovation. The latest software allows simple, fast and automatic transfer between different imaging techniques within multimodal systems and accurate co-registration of the images produced. In the future, increasing commonality in user interfaces across instruments looks set to allow researchers to switch more easily from one to another, saving time and reducing errors.
“A significant advance in preclinical imaging tools has been the introduction of multimodal animal beds, which are compatible with a number of instruments, removing any requirement to disturb the animal during a cross-platform study. When conducting analyses on a multimodal imaging system, this accurate positioning facilitates the layering of images to improve insight during subsequent study.”
Q: Can you share some specific examples for how optical imaging is used in studies?
“Imaging provides crucial datasets to scientists in a number of clinical areas including neurology, cardiology and metabolic disease. However, optical imaging technology combinations are being most effectively applied and are having significant impact in preclinical oncology research where they are strengthening the options for in vivo visualization of cancer-related processes over time. While different imaging modalities each offer particular benefits in oncology, of particular note is the use of imaging techniques to study tumour progression, to visualise molecular markers and for research into the mode of action of cancer therapeutics.”
“For tumour imaging and monitoring, BLI is well suited to longitudinal studies, due to its excellent signal-to-noise ratio (SNR). There is a strong positive correlation between measured BLI signal and actual tumour burden, which has been confirmed by tumour histology. In these instances, Genetic intrinsic FP (GFP) reporters enable imaging without the need for substrates or nearby metabolites as they present shallow and bright signals. For short-term, semi-quantitative FLI, tumour cells may be pre-labelled in culture using organic or inorganic fluorphores.”
“Interestingly, malignant tumour development requires an accumulation of mutations, which can be related to apoptosis regulation, cell adhesion molecule expression, and angiogenic and metastatic potential. These mutations can result in the production of unique molecular markers, which are visualized in preclinical in vivo studies by the use of probes. DRI is a valuable modality here, and is favoured over FLI, as radionuclides are small in comparison to fluorescent molecules and, therefore, less prone to modify small-molecule biodistribution. In addition, some radionuclide tracers can be imaged by CLI.
“Optical in vivo imaging can also be effectively leveraged for therapeutic response studies. BLI is employed in the evaluation of novel therapeutic agents, while FLI has been used extensively to track the biodistribution of traditional drug compounds and candidate drug delivery vehicles in vivo. As you can see, the technique is making a significant impact and has enormous future potential too…”
In conclusion
Rising global demand for efficacious, inexpensive medicines is fuelling increased activity throughout the drug development pipeline. Across the pharmaceutical industry, the drive to reduce costs and time to market for new products is putting evermore pressure on preclinical research to accurately inform efficient drug development and delivery processes. Clearly imaging is at the forefront of the revolution in preclinical information, providing increasingly valuable insights into disease mechanisms and progression. A range of imaging modalities are already being used to inform therapeutics in a number of clinical areas, most significantly in progressive disease research fields, such as oncology studies.
Technological advances are aiding the translation of preclinical research work from in vivo models into the clinical situation. The development of multimodal systems alongside state-of-the-art hardware and software is bringing new cross-platform capabilities, facilitating more accurate analyses and improved access to useful data and enabling higher test throughput. Looking forward, these innovations will surely put more powerful data into the hands of researchers, further accelerating the development of drugs and informing clinical practice.
For more than 50 years, Bruker has enabled scientists to make breakthrough discoveries and develop new applications that improve the quality of human life. Bruker’s high-performance scientific research instruments and high-value analytical solutions enable scientists to explore life and materials at molecular, cellular and microscopic levels. For more information, please visit: https://www.bruker.com/