French biopharmaceutical company PharNext SA is taking a different approach to drug development, by identifying new indications for novel combinations of off-patent drugs at low doses.
Xavier Paoli, chief commercial officer and vice president of R&D operations, said during an interview with Bioscience Technology at the BIO CEO and Investor Conference in New York City, that the company can cut five years off the drug development process using their new R&D paradigm called PLEOTHERAPY.
PharNext was founded in 2007 by scientists and entrepreneurs including Daniel Cohen, M.D., Ph.D., a pioneer of modern genomics, who co-founded the Jean Dausset Foundation (formerly known as the Center for the Study of Human Polymorphism (CEPH)) in 1984, and helped generate the first physical map of the human genome in 1993.
The drug discovery platform is based on genomic and other data that is analyzed to create what the company calls a complex biological disease network, which is essentially an inventory of potential therapeutic targets and drugs that might act on these targets.
Focusing first on neurodegenerative diseases that have no therapeutic treatments, or where options are not optimal, the company has an ongoing Phase 3 trial for Charcot-Marie Tooth Disease Type1A and has completed a Phase 2a study for Alzheimer’s disease.
Filtering to find treatments
While repositioning drugs is not new in the pharma industry, repositioning and combining drugs in a systematic way is, Paoli said. PharNext analyzes big data using statistical models, algorithms, and bioinformatics to pull all sorts of data – such as genomic, metabolic, and proteomic data – around one specific disease. It takes about one year to build this complex molecular network of the disease, which then identifies which targets might have an effect with potential drugs.
There are around 2,000 off-patent drugs that are available and once the disease network is developed it can be used, along with bioinformatics tools, to filter down to about 50 candidates, Paoli explained. Then those drugs are tested both alone and in combinations in vitro on specific cellular models of the disease for about one year. Results from the in vitro screenings usually further reduce the number of candidate drugs to about 25. From there the company identifies the best combination by lowering the dose and seeing which have a significant effect on a specific model. Based on that the company can identify three to four combinations for a disease that are then tested in animals, which then leads to one combination that moves into clinical development.
“So we select the combination based on several factors, the first one being the potential safety profile, but also the intellectual property that is available for these molecules,” Paoli said.
Typical drug development takes around 15 years, according to Paoli, but with PharNext’s process the time can be cut down to 10 years, as seen with their most advanced drug PXT3003, which anticipates a read-out from its Phase 3 data in the second quarter of 2018. The company is able to save time in preclinical development as well as during clinical stages because sometimes they are not required to conduct Phase 1 studies since the safety profile is already known.
Charcot-Marie-Tooth disease
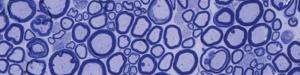
Charcot-Marie-Tooth disease (CMT) is a group of rare, hereditary, degenerative nerve diseases that usually appears in teenage years or early adulthood. The most common form of the disease is CMT type 1A (CMT1A), which is an orphan disease that affects at least 125,000 people in the U.S. and Europe. Patients experience muscle weakness, decreased muscle size and decreased sensation. In CMT1A people have a duplication of the PMP22 gene, and overexpression of this gene causes demyelination of the axons on peripheral nerves, leading to nerve degeneration.
Currently, there are no cures for the disease, and the most common treatment is physical and occupational therapy, as well as medications to reduce pain.
Using the PLEOTHERAPY platform, the company identified three molecules that might be efficient in treating CMT1A: baclofen, naltrexone, and sorbitol. The original indications included muscle spasticity in multiple sclerosis, opioid addiction and constipation.
“So you can you see that [these indications] had nothing to do with CMT1A,” Paoli said.
In preclinical work researchers were able to show that the PLEODRUG developed from these molecules, called PXT3003, was able to reduce overexpression of the PMP22 gene and improved CMT1A rat models on both clinical and non-clinical endpoints.
Then came a Phase 2A study of 80 patients in France. The double-blind, randomized trial had four arms: a low dose, intermediate dose, high dose and placebo arm, with 20 patients in each. The oral liquid formulation was given twice daily, and patients were followed for 12 months. Eleven endpoints were tested, with one being a score on the Overall Neuropathy Limitations Scale (ONLS) which measures the disability of a patient, as well as the Charcot-Marie-Tooth Neuropathy Score (CMTNS), which is a measure of the level of the severity of the disease and patient impairment.
Several functional measures were also tested, such as the six-minute walk test, and hand grip to measure the strength of the patient.
Results showed a clear dose effect between the three dose levels, and in the high-dose arm there were three endpoints that were statistically significant and significantly improved versus the placebo, Paoli said. One of these was the ONLS score, which is the primary endpoint that has been agreed upon by the Food and Drug Administration (FDA) and the European Medicines Agency (EMA) for the pivotal Phase 3 study. In the high-dose arm they observed an 18.6 percent improvement compared to the placebo, which is statistically significant. Paoli said that if the company is able to show at least two-thirds of the improvement that has been seen in Phase 2 on this endpoint, that the Phase 3 trial would be considered positive
In addition safety and tolerability results were positive, with zero difference between the placebo arm and therapy arms, Paoli said. Both the EMA and FDA granted Orphan Drug Status to the company’s rare disease drug.
In December PharNext completed enrollment of 323 patients at 30 sites across the U.S., Canada, and Europe, with mild to moderate CMT1A. All enrolled patients have a diagnosis of the disease that’s been confirmed by genetic testing. The results of the pivotal, randomized, double-blind trial are expected next year. Patients will either receive a placebo, the high dose of PXT3003 given in Phase 2, or a dose twice as high.
A new target in the fight against Alzheimer’s disease
PharNext’s Alzheimer’s disease drug, PXT864, has been tested in Phase 1 and Phase 2a clinical trials, and focuses on a new mechanism of action. Unlike many drugs in the industry, this therapy does not target amyloid-beta or tau protein, buildup of which is known to be a hallmark of Alzheimer’s.
“We think that at the origin of Alzheimer’s there is a disequilibrium in the patient brain between the excitatory and inhibitory pathway,” Paoli explained.
The excitatory pathway would be too activated, and the inhibitory pathway would be too inhibited. Because of this disequilibrium, due to a metabolism issue, the brain enters a vicious cycle where it stimulates the overproduction of amyloid-beta and amyloid-beta stimulates the imbalance between the excitatory and inhibitory phase, according to Paoli. PharNext’s mechanism of action is to act upstream of the amyloid-beta and tau protein.
“The idea with our combination is to break this vicious cycle and to restore the balance between excitatory and inhibitory phase,” he said.
In December the company presented positive exploratory Phase 2 Data from PXT864 at the 9th Clinical Trials on Alzheimer’s Disease (CTAD) Conference in San Diego. The results suggest that the drug, which is an orally administered combination of baclofen and acamprosate, is well tolerated and safe for use in patients with Alzheimer’s. It also may slow the progression of cognitive disability, as shown by the primary endpoint of the study, the AD Assessment Scale Cognitive Subscale test.
The company plans to conduct a Phase 2b study later this year to refine the dosing of the drug and to also test it in combination with the standard of care in Alzheimer’s which is donepezil.
Other neurodegenerative diseases may have similar origins and Paoli said the company has good preclinical data in models of Parkinson’s and ALS, so they would like to move into Phase 2a studies for those conditions as well.
If Phase 2a and Phase 2b trials produce strong results then the company would try to find a partner to perform Phase 3 studies.
A third arm of the company’s business model is to have R&D collaboration with big pharma or other biotech companies that want to rescue a drug. With their platform they can perform what is called reverse positioning, meaning that for a drug that failed in Phase 2 for example, because of a poor safety or efficacy profile, the technology can ‘rescue’ the drug either by identifying another indication or combining this molecule with other known drugs.
While the company doesn’t currently have the financial means to investigate a number of diseases, the platform is universal, said Chief Financial Officer Pierre Schwich, so PharNext potentially has a very large portfolio of other diseases that could develop in the future.