Simone T. Sredni, M.D., Ph.D., associate professor of pediatric neurosurgery at Ann and Robert H. Lurie Children’s Hospital of Chicago / Northwestern University Feinberg School of Medicine and member of Tadanori Tomita’s research group, has been working in pediatric brain cancer research for about 15 years.
In an exclusive interview with Bioscience Technology, Sredni said that after so many years in the field, she has “never felt so close” to finding a better treatment for atypical teratoid/rhabdoid tumors (AT/RT) —and the powerful gene-editing tool CRISPR/Cas9 helped her get there.
AT/RT are very aggressive and unresponsive tumors that most frequently develop in very young children, under three months old. This type of tumor is universally lethal and survival rarely exceeds two years, Sredni said.
The current treatment option involves about eight chemotherapy drugs, radiation when age permits, along with surgery. Even still, children die, so really there is no good treatment currently available, Sredni explained.
“My main focus is to find new and less toxic treatments for these children,” Sredni said.
So, the idea came about to screen the kinome, which is the complete set of protein kinases encoded in the genome.
“Kinases are good therapeutic targets because they are involved in many cellular functions including proliferation and survival, and they can be targeted using inhibitors,” Sredni said.
Investigating the kinome
Sredni had the opportunity to beta test Thermo Fisher Scientific’s LentiArray CRISPR human kinase library and was able to functionally inactivate 160 kinases, which correspond to one-third of the whole kinome.
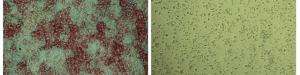
So her team mutated each one of the 160 kinases in a cell line derived from one of the very aggressive pediatric tumors and observed that mutations in 5 percent of them significantly impaired cell proliferation.

They found that the protein kinase called Polo-like kinase 4 (PLK4), which is increased in AT/RT, regulates these tumors’ growth, survival and tendency to metastasize.
Interestingly, Sredni had performed a number of genomics studies previously, and this specific marker had never popped up before.
“If I hadn’t done this functional study, where, knocking out the PLK4 gene, resulted in the inhibition of cell proliferation I wouldn’t have discovered that PLK4 is essential for AT/RT growth. PLK4 is only slightly elevated in these tumors. However, this is gene is tightly regulated and slight increases in its expression results in an aggressive tumor phenotype. This overexpression can be targeted by inhibitors opening a new therapeutic prospective for children with AT/RT. Significantly, we also found it elevated in other embryonal tumors of the brain, what may have a larger impact in patient care,” Sredni said. “The fact that we used CRISPR for the functional assay was key.”
Even more promising, Sredni and her team were able to target the kinase with an available PLK4 inhibitor currently being tested for breast cancer that so far is “providing promising results.”
Sredni’s group experiments showed that the drug significantly impaired AT/RT cell proliferation, survival, migration and invasion.
More interestingly, it appears that the drug does not affect normal cells. The researchers tested the toxicity of the drug in normal human fibroblasts and in zebrafish larvae, exposing them to high doses of the drug for extended periods of time and found that it did not affect the fibroblasts and did not increase death or affected development of zebrafish larvae. This is a sign that the drug may be safe for use in pediatrics.
The team has now moved on to studies in mice with intracranial xenograft. While this is still under development, Sredni said it looks like tumors are actually growing significantly slower or even shrinking.
“So I’m knocking on wood here and hoping for good news soon” she said.
CRISPR’s reach
CRISPR made a big impact on this research and Sredni, like many, think the tool’s reach will be broad.
“The advent of CRISPR— I think it’s going to change science from now on, in every aspect,” she said. “It’s really user-friendly, robust and reliable.”
“Of course it’s not perfect, it still needs some optimization,” Sredni acknowledged. “But, it is powerful! For example in my hands, with a small team and the help of my summer students, we were able to mutate individual kinases, observe the cells’ phenotype and make significant new discoveries.”
While she thinks progress in therapeutics will be more challenging than discovery, she added, “CRISPR will really make a difference in what we will be doing from now on in cancer research.”
Next, Sredni will perform high-throughput analyses on her mutated and treated cells in order to find downstream targets that will be adequate for combined therapies.
“One drug alone won’t cure cancer,” she said.
The team is working on developing data for an application for federal funding in order to fully characterize the phenomenon observed so far. If all goes well, Sredni sees a Phase 1 clinical trial coming up soon.
The findings were published in Pediatric Blood & Cancer.