Training T Cells to Fight Their Own Cancers
 Immunotherapy—the art and science of training peoples’ immune systems to fight their own cancers—was named Breakthrough of the Year by Science.
Immunotherapy—the art and science of training peoples’ immune systems to fight their own cancers—was named Breakthrough of the Year by Science.
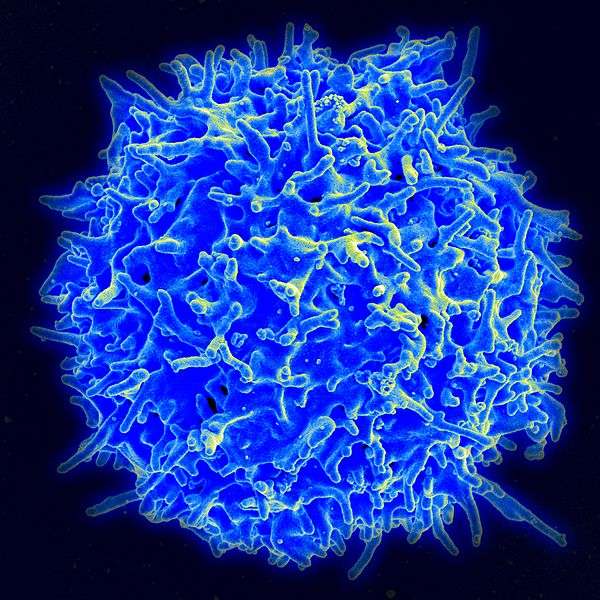
Prominently mentioned was an approach seeing unprecedented success in the clinic: genetically tweaking patients’ own cancer-fighting T cells to make them more potent, proliferative, and targeted. The two major types of T cells being engineered this way are called CARs (chimeric antigen receptors) and TCRs, or antigen-specific T Cell Receptors.
In recent months, such T cells have proved unusually effective at attacking antigen, or molecular sites, specific to acute and chronic lymphoblastic leukemias, and melanomas. In a particularly hailed coup, the teams of the University of Pennsylvania’s Carl June, and Memorial Sloan Kettering’s Michel Sadelain, reported to the American Society of Hematology (ASH) that 45 of 75 leukemia patients saw complete regressions with CARs.
Science called the CAR response “eye-catching,” and contended that clinical trials this year “have cemented” cancer immunotherapy’s “potential in patients and swayed even the skeptics.”
“We now know we can make potent T cells from patients’ blood cells,” Sadelain tells Bioscience Technology.
 The CAR/TCR approach has been so successful that in 2014, genetically engineered T cells will move into clinical trial for more cancers. The trials will be sponsored by, among others, the labs of Steven Rosenberg of the National Cancer Institute (NCI), June, Sadelain, and—most unusually for immunotherapy—the pharmaceutical giant, Novartis.
The CAR/TCR approach has been so successful that in 2014, genetically engineered T cells will move into clinical trial for more cancers. The trials will be sponsored by, among others, the labs of Steven Rosenberg of the National Cancer Institute (NCI), June, Sadelain, and—most unusually for immunotherapy—the pharmaceutical giant, Novartis.
In a 2006 issue of Science, Rosenberg, NCI Chief of Surgery, published the first clinical paper on genetically engineered TCRs. They were given to melanoma patients. In 2010, Rosenberg published the first CAR paper showing clinical responses in lymphomas via the antigen so successfully targeted by June and Sadlain: CD-19. The methods evolved out of the successful tumor infilatrating lymphocyte (TIL) approach, finessed by Rosenberg. TILs are T cells collected from patients' melanoma tumors--thus, the most naturally successful anti-cancer T cells mustered by the patients' bodies. The cells are captured; expanded to great numbers; reinfused.
“When it comes to TILs, you can generate T cells unique to that cancer and no other cancer,” says Rosenberg. “In one of our melanoma clinical trials with TILs, 40 percent of patients experienced durable complete tumor regressions lasting beyond five years. It’s incredible.”
But TILs so far only work for melanoma tumors. This is partly because it takes special labs weeks to make them; partly because not all tumors are so immunogenic they naturally attract enough T cells to work with. Cells made into CARs and TCRs are simply culled from the blood, so they are less naturally targeted than TILs. But they are genetically tweaked into shape. They take less time to make. And no surgery is required for retrieval. So Rosenberg is accruing patients for eight CAR and TCR trials with many cancers, including epithelial, colorectal, lymphoma, kidney, glioblastoma, pancreatic, and mesothelioma.
The CAR therapy of June and Sadelain that has been attracting so much attention involves attaching parts of antibodies to patients’ T cells. The result is cells with the impressive homing abilities of antibodies, and the killing skills of T's. The teams' most hailed CARs recognize and attack the key CD-19 antigen on the surface of acute lymphoblastic leukemia (ALL) cells. In one trial, 19 of 22 children who had exhausted all drug treatment and bone-marrow transplant options for ALL went into remission after receiving that particular therapy, now known as CART-19, according to data presented at ASH. Only five patients later relapsed.
In CLL, CART-19 saw a response in 47 percent of patients, with half of those experiencing a complete remission.
CART-19 is the first therapy to work on such patients after they have failed bone marrow transplants. Novartis has licensed the technology, and has spent $43 million on labs to develop the approach. It plans a large ALL trial in 2014.
CARs and TCRs possess different pros and cons. As noted, TCRs involve genetically tweaking T cells to make them more potent. A main drawback: they must follow the rules of T cell immunohistochemical recognition, so can only target certain cells. As CARs are part antibody, they don't follow T cell recognition rules. So CARs can go after a wider variety of tumor cells. But TCRs can go after targets both within cells and on cell surfaces, whereas CARs can only go after targets on cell surfaces.
The major drawback of both: very few targets have been found specific only to tumors. This is critical. T cells can cause massive collateral damage when they attack targets found on both tumors and healthy cells.
 “Finding the right target antigen for a number of cancers, beyond the very successful case of acute lymphoblastic leukemia, is a major future goal for our field,” says Sadelain. “An ideal target would be abundant in the tumor and absent from normal cells, but few molecules recognized by CARs and CCRs meet this requirement. We need to more extensively study the surface of tumors to find adequate targets that suit the CAR technology. We also need to design smarter T cells that can discriminate between tumor cells and normal cells.” CCRs are chimeric co-stimulatory receptors. By engineering T cells to target two antigen on tumors at once--via both a CAR and a CCR--even more precision can result.
“Finding the right target antigen for a number of cancers, beyond the very successful case of acute lymphoblastic leukemia, is a major future goal for our field,” says Sadelain. “An ideal target would be abundant in the tumor and absent from normal cells, but few molecules recognized by CARs and CCRs meet this requirement. We need to more extensively study the surface of tumors to find adequate targets that suit the CAR technology. We also need to design smarter T cells that can discriminate between tumor cells and normal cells.” CCRs are chimeric co-stimulatory receptors. By engineering T cells to target two antigen on tumors at once--via both a CAR and a CCR--even more precision can result.
Sadelain’s group published a paper in Science Translational Medicine this month offering suggestions along those lines. His group plans CAR trials next year for lung, ovarian, and prostate cancers.
Rosenberg agrees that “the critical issue is the paucity of tumor-specific antigen” shared by tumors from large numbers of patients. But because cancers are so heterogenous, the final answer may lie, he says, in fully assessing each individual’s unique tumors, and devising T cells specific to those alone, patient by patient. His team is working on this highly personalized approach, as well.





