Patient-relevant Preclinical Models Using Image-guided Small Animal Irradiation
 Radiotherapy is a primary, adjuvant or neoadjuvant treatment for a number of different cancers, such as glioblastoma, breast, lung and prostate. It is part of the treatment regimens for the majority of cancer patients worldwide. Significant advances have been made in improving the delivery of ionizing radiation to provide precise dosing with reduced side effects to surrounding normal tissue using image-guided micro-irradiation (IGMI). Image-guided radiation therapy (IGRT) is also used to reduce the amount of radiation delivered to the normal tissue surrounding the targeted tumor. However, in the preclinical setting, the use of IGRT is less common. Traditional irradiation studies utilize whole body irradiation with lead shielding, attempting to focus the radiation to a specific area on the animal.
Radiotherapy is a primary, adjuvant or neoadjuvant treatment for a number of different cancers, such as glioblastoma, breast, lung and prostate. It is part of the treatment regimens for the majority of cancer patients worldwide. Significant advances have been made in improving the delivery of ionizing radiation to provide precise dosing with reduced side effects to surrounding normal tissue using image-guided micro-irradiation (IGMI). Image-guided radiation therapy (IGRT) is also used to reduce the amount of radiation delivered to the normal tissue surrounding the targeted tumor. However, in the preclinical setting, the use of IGRT is less common. Traditional irradiation studies utilize whole body irradiation with lead shielding, attempting to focus the radiation to a specific area on the animal.
The deployment of innovative technologies and the translation of laboratory findings for human treatment must be supported by rigorous preclinical studies. Research into radiation therapies has continually been held back by a lack of reliable orthotopic tumor models for researchers to target. Preclinical studies of new radiation treatment methods have been difficult due to the technological inequality between the simple methods for laboratory animal irradiation and those for advanced human treatment. Realizing this drawback, scientists and researchers developed specialized radiation delivery systems with precision suitable for laboratory mice and rats, which will deliver irradiation to a localized region in the mouse and keep healthy tissue damage to a minimum. It has also created a demand for a more predictive model that will closely reflect the human microenvironment and improve knowledge of which therapeutic approach would work best for a given patient.
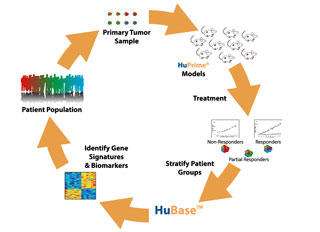
Using human-derived cancer models alongside radiation delivery will assist scientists is gaining a better understanding of treatment response at a genetic level. Patient-derived xenograft (PDX) models are in vivo animal tumor models established directly from patient tumor samples, without any in vitro manipulation, to more closely mimic the clinical situation for patients in the preclinical setting and help improve potential cancer treatment regimens. It has been shown that these tumor xenografts maintain essential histopathological features and genetic profiles of the original patient tumors and are the most clinically relevant animal models for cancer drug discovery. These models enable many different combinations of molecular and radiation therapies to be tested, therefore allowing oncologists to devise the best therapeutic regimens for each patient, making personalized medicine a reality.
Radiation therapy is part of the treatment for most cancer patients. Therefore, providing preclinical models that more closely reflect a patient’s condition should be a potential option for validating the efficacy of novel therapies and potential compounds that make tumor cells more sensitive to radiation therapy (radiosensitizers) for cancer treatment. The use of the IGMI technique in conjunction with a radiation therapy platform will provide a unique portfolio of models that closely mimic the treatment regimen in the clinical— only in a preclinical setting.
High-resolution imaging enables researchers to pinpoint an exact clinical target and deliver a precise radiation dose to in vivo and in vitro models. The platform provides the ability to perform combination studies in PDX models and cell line-derived xenograft (CDX) models, as well as in vitro, in addition to irradiated subjects for hematological models.
The development of an image-guided small animal radiation research platform allows for a more accurate treatment of animal models of cancer, and more importantly, for planned protocols similar to those utilized in the clinic. This platform integrates cone beam computed tomography (CBCT) imaging (high-resolution, low-imaging dose and 3-D reconstruction) with radiation treatment (X-ray). Non-copular field arrangements and anterior posterior/posterior-anterior irradiation is enabled via a chamber that incorporates a gantry and robotic specimen stage, where the irradiation and imaging takes place.
The image-guided small animal radiation research platform is a portable and customizable platform that incorporates high-resolution computerized tomography (CT) imaging with precise radiation delivery, assisting researchers to pinpoint and deliver 0.5 mm beams to an exact anatomical target. It is designed to close the gap between current clinical techniques and radiation biology/radiotherapy, enabling researchers to confidently assess the efficacy and efficiency of current treatment regimens, while providing new data to the medical community that can assist in shaping the future of radiation protocols and concurrent therapies. This dramatically changes the issue of radiation damage to healthy tissue surrounding the targeted tumor. The high-resolution CT imaging identifies exact tumor location, while the 0.5 mm beams can be delivered to a precise anatomical target.
Through the use of PDX models, in conjunction with radiotherapy, preclinical testing can predict which patients would benefit from combination therapy, which cancers would be more radio-resistant and whether that particular patient is a candidate for molecular targets. With the use of today’s equipment, it is possible to mimic what occurs during treatment. Radiobiologists are able to determine how radiation is interacting with the tissue surrounding the tumor, while also observing the mechanisms and the DNA damage and repair that arise during radiation.
The image-guided small animal radiation research platform allows the use of irradiation with anti-cancer agents in small animals with reduced side effects and improved outcomes. This will allow these preclinical models to be used effectively for drug discovery programs to identify promising treatment options for clinical testing of cancer models using either radiotherapy alone, or in combination with new agents.
The future of anti-cancer treatments lies with both radiation and combination therapies. Instead of a primary chemotherapy/radiation therapy approach, treatment should be combined and based on both the patients’ genome and their individual cancer. Through varied combination therapies, resistant cells will become less likely, and through preclinical PDX model research, the combination of the therapy becomes targeted and personal, elevating the patients’ chance for survival.

