A Fascinating Year in Breast Cancer Advances
 Some of the most important advances in breast cancer this year were related to all kinds of heterogeneity: within tumors, between tumors in a single patient, and between tumors in early and later stages, according to oncologists speaking at conferences, and contacted by Bioscience Technology.
Some of the most important advances in breast cancer this year were related to all kinds of heterogeneity: within tumors, between tumors in a single patient, and between tumors in early and later stages, according to oncologists speaking at conferences, and contacted by Bioscience Technology.
“This year we had a lot of fascinating stories,” Jorge Reis-Filho told the San Antonio Breast Cancer Symposium in December. Reis-Filho is a cancer geneticist at Memorial Sloan Kettering Cancer Center. Among the most important stories, he said, was the repeated confirmation, due to improving technology and massive genetics projects, that “heterogeneity is incredibly prevalent.”
Other areas of note, said oncologists, included findings that PALB2 is a strong germ-line proclivity gene; that drugs can be added to Herceptin to increase its potency; that ovarian suppression can work on some populations; and that long-term tamoxifen can prompt estrogen-induced apoptosis.
PALB2
Daniel Hayes, a University of Michigan Cancer Center oncologist, told Bioscience Technology that one of the great papers of 2014 involved “identification of germ-line inherited mutations other than BRCA1 and 2 that increase susceptibility/risk for breast cancer.” The New England Journal of Medicine (NEJM) paper, by Addenbrooke’s Hospital’s Marc Tischkowitz, found that patients with a mutation in the PALB2 gene stand a one in three chance of getting breast cancer by age 70. The gene interacts with the deadly BRCA1 and BRCA2, and has been called the potential “BRCA3.”
 Reis-Filho noted the study included 154 families from 14 centers, with PALB2 loss-of-function germline mutations. Of 311 women, he said, 229 got breast cancer. Of 51 men, seven developed cancer.
Reis-Filho noted the study included 154 families from 14 centers, with PALB2 loss-of-function germline mutations. Of 311 women, he said, 229 got breast cancer. Of 51 men, seven developed cancer.
Like BRCA, he said, the risk increased with age, until at 70, the risk was 35 percent. This is modified by family history—if at age 50 one has no family history, the risk is 13 percent. But with strong family history, the risk increases to 60 percent.
“It is fair to say we now have yet another high-risk gene for breast cancer development in the form of PALB2,” said Reis-Filho. “The increased risk of breast cancer is probably similar to that of BRCA mutations. It should be added to genetic testing panels. This should not be too much of a problem because several centers are now using multi gene panels to sequence patients for breast cancer risk.”
Clinical advances
One of the year’s biggest clinical advances was outlined in an upcoming paper by Medstar Washington Hospital Center’s Sandra Swain. The paper will demonstrate that “combination trastuzumab (Herceptin) and pertuzumab (Perjeta), with chemotherapy, increases overall survival compared to chemo and trastuzumab alone in Her2 metastatic breast cancer,” Hayes told Bioscience Technology. A 2014 abstract related to the paper found that patients on the above combo lived 16 months longer.
Another big clinical advance, according to Hayes, was outlined in an NEJM paper demonstrating “that for selected premenopausal women with ER+ early stage disease but relatively higher risk for recurrence, ovarian suppression or ablation plus aromatase inhibition (AI) [exemestane] is superior to Tamoxifen alone.”
Hormone therapy resistance
In the ever-evolving area of hormone therapy resistance, further confirmation of last year’s lauded papers finding that ESR1 confers resistance to aromatase inhibitors was achieved. One particularly notable confirmation came in the form of a 2014 Annals of Oncology study by Gustave Roussy oncologist Monica Arnedos, which found that as breast tumors progressed in patients from the SAFIR01 and MOSCATO trials, “only one gene crashed the party” in later stages— “and that is ESR1,” said Reis-Filho. Other tumor genes increased in frequency.
Differing tumor evolution speeds
Nick Navin, using his new single-cell, dual-purpose nuc-seq technology, showed in Nature this year that chromosome rearrangements and copy number variations occur in triple negative (TN) and estrogen receptor positive (ER+) breast cancers “early and in punctuated bursts of evolution,” Reis-Filho said. Meanwhile, nuc-seq showed that, by contrast, “point mutations are acquired in a gradual manner.” Navin is an oncologist at MD Anderson Cancer Center.
Size doesn’t matter
Kornelia Polynk of Harvard University revealed, in another 2014 Nature study, that minor sub-clones can be cooperative and indeed end up driving a tumor, Reis-Filho said. This year, he said, oncologists learned that the field should not “overlook minor subclones. Some cooperate, they do not just compete. They can have functional significance and should not be ignored just because they exist at low frequency. Of course, how to ID these clones remains a big challenge.”
The bottom line, said Reis-Filho: “Intra-tumor heterogeneity is common.”
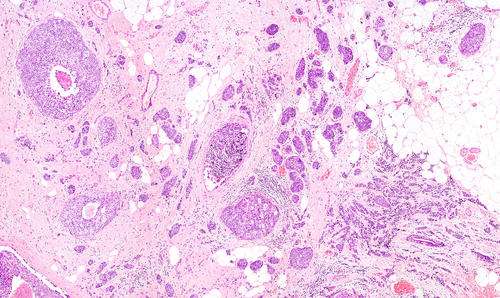
TILs matter—a lot
This year, two groups confirmed that lymphocytes that enter tumors—natural tumor infiltrating lymphocytes (TILs)—can tip the balance between the deadly and the curable. Peter McCallum Cancer Centre oncologist Sherene Loi earlier took on the “Herculean task” of quantifying all the TILs in tumors in the BIG 02-98 trial, said Reis-Filho. In the Journal of Clinical Oncology she showed that post-chemotherapy, triple-negatiive breast tumors consisting of 50 percent TILS “had incredibly good outcomes, overall survival of 92.3 percent.”
This was confirmed by the New York University Cancer Institute’s Sylvia Adams this year in the Journal of Clinical Oncology.
“These two studies provide evidence for stromal lymphocytes being a prognostic indicator for TNBC patients on chemotherapy,” said Reis-Filho. Another 2014 Loi study, in Annals of Oncology, also found that there was a “significant interaction between TILs and Herceptin in Her2 positive patients. This was consistent with the notion that pre-existing host antitumor immunity would be important for trastuzumab (Herceptin) efficacy. That was really exciting.” That study was cited as one of 2014’s best in Annals of Oncology.
However, he said, preliminary evidence presented by the Mayo Clinic’s Edith Perez at the San Antonio conference cast some doubt on the Herceptin finding. “We have a big, big challenge here,” he said. “If we are to use quantification of TILs as a marker, we have to standardize the methodology for the assessment thoroughly.”
Happily, he added, guidelines for quantification have been devised by Loi and others. “We recommend all pathologists to read these in detail. This needs to be ‘pitch perfect.’ We need to characterize TILs in detail in order to guide us whether patients should be on immune checkpoint inhibitors, among other therapies, for TN and Her2 positive cancers.”
 Apoptosis due to long-term Tamoxifen
Apoptosis due to long-term Tamoxifen
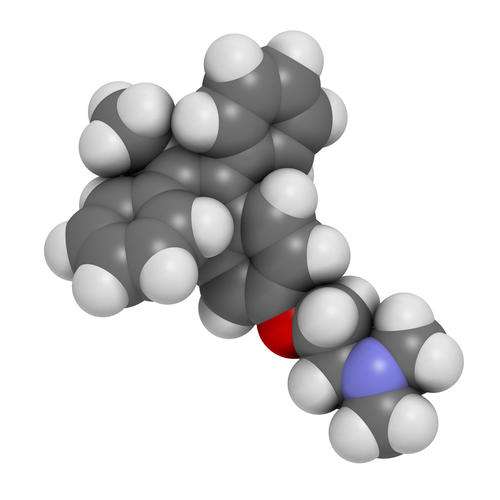
Tamoxifen made headlines again. Widely hailed was the news that the American Society of Clinical Oncology (ASCO) and other cancer societies changed their recommendation for use, for many hormone positive patients, from five years to ten.
Breast cancer and the WHI
And a Cancer Research paper by MD Anderson oncologist Craig Jordan, given a three-star “exceptional” rating on F1000Prime, attracted attention.
That paper offered an explanation for why the Women’s Health Initiative (WHI) study, which gave hormone replacement therapy (HRT) to post-menopausal women, resulted in an increase in breast cancers. The synthetic progestin in the Wyeth drug, medoxyprogesterone acetate (MPA)—which is not physiologic—blunts estrogen-induced cancer cell apoptosis (cell death) in vitro, Jordan’s group said in the paper. Meanwhile, an HRT alternative, called norethisterone acetate (NETA), did not.
Henry Burger, emeritus director of the Prince Henry’s Institute of Medical Research wrote: “The findings have important therapeutic implications, suggesting that it may be preferable to use NETA in hormone therapy, rather than MPA.”
Jordan told Bioscience Technology that NETA is an "oral contraceptive that has been used safely for 50 years by millions of well women. Unlike MPA, which has a glucocorticoid complication that stops the estrogen in HRT from causing apoptosis of estrogen-deprived occult breast cancer in post-menopausal women, NETA is a synthetic progestin with an associated estrogenic property that adds to the killing of breast cancer cells, while protecting the postmenopausal uterus.”





