Cord Blood Stem Cells Increased Tenfold
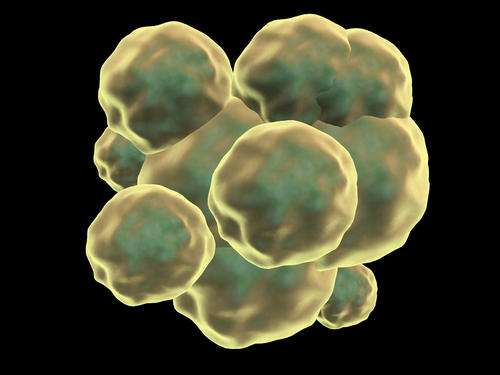 Ten times more stem cells can be generated from umbilical cords than ever before, according to a new Science study.
Ten times more stem cells can be generated from umbilical cords than ever before, according to a new Science study.
The potential advance was made via a little-known pyrimidoindole molecule called UM171. Tested by the team of University of Montreal investigator Guy Sauvageau, UM171 may dramatically reduce blood (hematopoietic) stem cell (HSC) transplant complications, and considerably increase patient access to the procedure. That molecule and others have been infusing the blood stem cell transplant field with excitement.
“Intriguing data,” University of Minnesota cord blood stem cell expert John Wagner told Bioscience by email. Wagner, uninvolved in the study, just finished a clinical trial of a competing molecule, SR1. The UM171 study offers “proof of concept that this new molecule has tremendous potential value in expanding hematopoietic stem cells (HSC) or primitive progenitors or both.”
“A notable advance,” said University of Toronto Program in Cancer Stem Cells Director John Dick. Also uninvolved in the study, he said UM171 so far appears to offer a “much more substantial expansion than the prior work on SR1 alone.”
Former NIH Director of the Center for Regenerative Medicine Mahendra Rao is also intrigued. Also uninvolved, he has written and talked about using cord blood stem cells for banks of induced pluripotent stem cells (iPSCs). This could make available, to most patients, potent stem cells that match their tissue types. For cord blood cells convert to embryonic stem cell-like iPSCs more efficiently than other cells.
“Exciting,” Rao said via email.
Notoriously difficult to expand
HSC transplants have been successfully used for decades to combat blood cancers and other blood disorders. Most HSCs are donated by adults. But in recent years, cord blood cells have proven superior to adult HSCs in a key way: they are less likely to be rejected by patients for whom there are no immunologically matched adult cells. Stem cells from umbilical cords are more naïve. Less immunological matching is necessary.
Cord stem cells also possess fewer genetic mutations than adult blood stem cells. They are “pristine,” as Rao has put it.
Finally, as noted, robust iPSCs are more easily made from cord cells.
Still, it has been notoriously difficult to expand, in a dish, both adult HSCs and cord stem cells. This has severely limited the number of patients able to benefit. Double cord blood transplants help. But while producing respectable hauls of short-term progenitors, long-term HSCs are not generated as quickly.
“Unfortunately, most expansion systems available to date achieve progenitor cell expansion at the expense of the LT [long-term]-HSC loss, increasing the risk of late graft failure,” the authors wrote.
UM171 vs. SR1
For the new study, investigators from the Universities of Montreal and Toronto screened many molecules. UM171, abandoned in a different study, was fortuitously tried.
From cord cells, UM171 prompted the production of blood cells that more expertly reconstituted the bone marrow of immune-compromised mice than other molecules tried— including SR1, which Wagner is using in clinical trial.
Wagner, director of the University of Minnesota’s Division of Blood and Marrow Transplantation, said by email: “This is an elegant study where the investigators systematically evaluated a new class of small molecules that expand the population of long-term repopulating HSCs in culture, as well as SCID-repopulating cells in immune-deficient NSG [Nod scid gamma] mice. They compare UM171 to SR1, an aryl hydrocarbon receptor antagonist, previously shown to expand primitive progenitors by a different mechanism.”
While noting UM171’s “tremendous potential,” he cautioned "the only true test is doing the transplant in humans” as he has done with SR1 with “extraordinary” results. (That paper is under review at a journal.) “And while the NSG murine recipient may be the best we have, it too has not been validated as the true test for the HSC.”
Still, he said: “I’m very interested in seeing this new molecule develop. Some would argue that we want to expand both HSC and progenitors in order to speed the time to neutrophil and platelet recovery. If we expanded only HSC, it might enhance engraftment, but time to recovery might still be long. Recall that after a cord-blood transplant, the median time to neutrophil recovery is 25 days with engraftment occurring in about 90 percent. In contrast, after adult peripheral blood stem cell transplant, time to recovery is 11 days in about 99 percent. While cord blood has many advantages, this is the most important challenge. Therefore, we are looking for progenitors and stem cells. Not one, but both. “
But can UM171 do this? “The preliminary data look encouraging,” Wagner said. “Is it better than SR1 or other methods in our clinical trials? Maybe, but only time will tell. It needs to be explored further. It’s an exciting time because it seems that the engraftment hurdle with cord blood may have been overcome.”
SRI “appears safe, and provides rapid recovery and sustained engraftment. Could UM171 be better? I don’t know. These results are exciting and worth further investment.”
University of Minnesota Stem Cell Institute Associate Director Dan Kaufman agreed. Also uninvolved in the new study, he said by email it is “interesting,” if “it is hard to say how much better/different than the SR1 agent used for comparison... SR1 is an aryl hydrocarbon receptor antagonist identified by Novartis to expand human HSCs (cord blood CD34+ cells) and published in Science in 2010 (Ref. 7 in the new paper)….While this new compound is reported better than SR1 in this new paper (and combined, seems even better), the studies are by two different groups, so it is not clear how much better one is.”
The takeaway: there are “many promising studies on HSC expansion moving into clinical trials. We are doing SR1. Leonard Zon [Harvard University] is doing PGE2. Irv Bernstein [Fred Hutchinson Cancer Research Center] is doing notch-mediated expansion. All seem promising in early trials. It remains to be seen how broadly applicable these strategies will be. UM171 is a late comer. If truly better, hopefully someone will test it in clinical trials.”
UM171 in clinical trial
Someone is. A UM171 clinical trial launches in December at the Maisonneuve-Rosemont Hospital. Sauvageau— who led the pre-clinical work— is also a hematologist at the Maisonneuve-Rosemont Hospital. The trial will last a year.
Dick noted Sauvageau’s work offers “a very robust set of data using the latest phenotypic markers, and importantly robust in vivo repopulation assays using gold-standard xenograft assays. While time will tell, I imagine it will be useful for adult HSC sources. More broadly, it opens the way to understand how HSC self-renewal is regulated.”
It is indeed possible cord stem cell yields could improve ten times over, Dick concluded. “If the xenograft assay represents a reliable reflection of what will happen in humans, this should be possible…Parallel analysis of an expanded unit in xenograft assays, as well as in clinical trial, will provide a valuable evaluation of how reliable the surrogate NSG repopulation assay is.”

