The Future of Treatments for Spinal Cord Injury
 There may be hope to get millions of individuals with chronic spinal cord injury (SCI) moving again, according to research presented at a press conference at Neuroscience 2014, the 44th annual meeting of the Society for Neuroscience (SFN) in Washington, D.C.
There may be hope to get millions of individuals with chronic spinal cord injury (SCI) moving again, according to research presented at a press conference at Neuroscience 2014, the 44th annual meeting of the Society for Neuroscience (SFN) in Washington, D.C.
Spinal cord injury often causes paralysis below the level of injury, and, as their injury becomes chronic, patients can suffer from secondary ailments such as urinary tract infections, respiratory issues and depression. There is no cure for SCI, so the new research— which includes a brain-machine interface that helps paralyzed patients walk again— is welcome news for those in need of a better quality of life.
“In some parts of the world, a spinal cord injury is a sentence of death,” said moderator Oswald Stewart, Ph.D., of the University of California, Irvine. “People with spinal cord injuries continue to live with various disabilities, ranging from the inability to walk, inability to use one’s hands, inability to breathe— and these are huge impacts on quality of life. Especially the loss of breathing ability.”
New brain-machine interfaces
In human research, Duke University’s Miguel Nicolelis, M.D., revealed groundbreaking details on a brain-machine interface that helps paralyzed patients walk again. The idea, which Nicolelis and a colleague introduced about 15 years ago, is aimed at developing “a potential new therapy for neuro-rehabilitation of patients suffering from devastating levels of body paralysis,” he explained.
At the SFN press conference, Nicolelis showed pictures and video of patients in an international study wearing what he dubbed a “whole-body exoskeleton”— a 165-pound brain-machine interface that acts as a wearable prosthetic suit. The 15-degree of freedom exoskeleton looks like a robotic vest, but it actually can controlled by brain-derived signals. The suit supports the weight of the person inside, is powered by hydraulics for “smoothness of movement” and is operated by a brain-machine interface (via an electroencephalography [EEG] cap).
“So, if you’re a paralyzed patient, you can basically dress [in] this device and use it to move again,” he said. “One of the main components…is the artificial skin. This is a flexible, printed circuit board that can be put together in a mesh, and [is] distributed to very key locations of the exoskeleton, like the surface of the foot, or the knees, or the hip, so that when the subject learns to walk, [they] can get feedback back from the exoskeleton to [their] body. We…fool the brain of the subjects to a point in which they feel that it’s not a machine that is carrying them, but [that] they are actually walking by themselves.”
The eight participants followed a staggered training regimen, which began with initial visualization coaching, until they could dictate specific movements to the system, such as walking and kicking. Eventually, participants were even able to feel what Nicolelis called “phantom limb sensation.” He explained that certain patients experienced such vivid phantom sensation that they reported feeling specific tactile feedback, such as walking on sand or blades of grass.
This technology has gained worldwide recognition. In June, one of Nicolelis’ study participants used the system to deliver the inaugural kick during the opening ceremony of the 2014 FIFA World Cup in Brazil. This participant helped Nicolelis’ team see one of the system’s most “stunning” advantages: some patients experienced neurological recovery.
“The patient chosen to actually take a kick in the World Cup had a T4-level [injury],” Nicolelis said at the SFN press conference. “But after seven months, when we reevaluated the patient, he could feel tactile stimulation up to T10. So he had a recovery of sensation six segments below the regional level.”
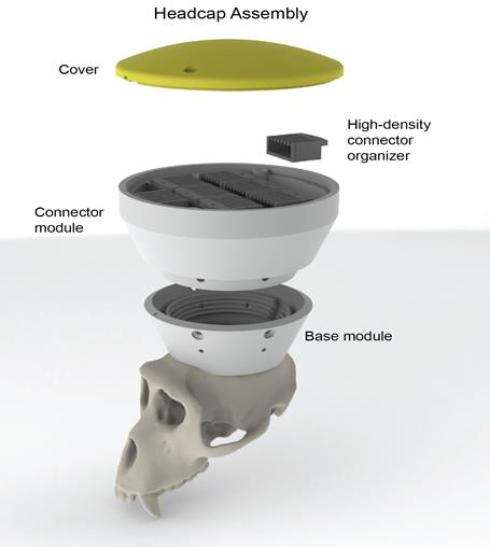
Additionally, Nicolelis is working on an implantable brain-machine interface, a “brain pacemaker” that is currently being tested in rhesus monkeys. The animals can control the movements of a motorized wheelchair “without performing any movement,” he said— just by thinking.
Nicolelis said this type of brain-machine interface is what “the future will bring to us, when we go from the surface of the brain [to the] inside [of] the brain, and use modern wireless technology…[to] record thousands of brain cells simultaneously and, in fact, create a brain-machine interface from inside the brain.”
Restoring respiratory function
 Indeed, loss of respiratory function is the main cause of death among people paralyzed by high spinal cord injury— and Phillipa Warren, Ph.D., of Case Western Reserve University, presented findings that may help patients draw breath long after spinal cord injury.
Indeed, loss of respiratory function is the main cause of death among people paralyzed by high spinal cord injury— and Phillipa Warren, Ph.D., of Case Western Reserve University, presented findings that may help patients draw breath long after spinal cord injury.
Warren’s research repaired paralyzed respiratory muscles in an animal model one-and-a-half years after spinal cord injury using a combination of enzyme injection with physical respiratory rehabilitation, in which researchers encouraged animals to breathe stronger and faster by putting them in slightly lower oxygen conditions. This behavior triggers respiratory nerves and strengthens the system.
“Breathing is essential to life. But over 70 percent of patients with spinal cord injuries have some degree of respiratory distress. This is often incredibly severe and they require some degree of ventilatory support,” Warren said at the press conference. “It reduces their quality of life and it increases their rate of mortality.”
Spinal cord injuries that occur very high in the neck region cause paralysis in all the muscles below, including the intercostal and the diaphragm. The muscles are part of the respiratory motor system, which Warren said to think of “as a circuit.”
“You have impulses from your brain which travel down your spin in a nerve, which connect to another nerve, which leaves the spinal cord and go to your diaphragm and innovate it, which [then] enables the muscle to contract, enabling you to breathe,” she said. “But following an injury that circuit breaks. Those impulses cannot get to your diaphragm and it is permanently paralyzed.”
With this in mind, Warren’s team attempted to not only find a treatment for spinal injury-induced respiratory paralysis, but to specifically try repairing that injury long after it had taken place. “Over time, the environment of the spinal cord changes, your problems change, and that means that your treatment strategy needs to change,” she said.
Fortunately, the combined treatment using an injectable enzyme (chondroitinase-ABC) was a winner. Even when the chondroitinase, which acts to strengthen the connections between nerves, caused an overabundance of molecules and unstructured activity within the diaphragm (erratic muscle activity), the team was able to provide a drug treatment to slightly reduce serotonin levels and eventually achieve regular breathing activity in the animals.
“What we’ve shown is that one-and-a-half years after injury we can recover respiratory paralysis, enabling normal, functioning breathing to occur,” Warren said. “While the treatment strategy requires optimization, this holds great promise for the future, and certainly [for] patients with spinal cord injury.”
Generating new nerves
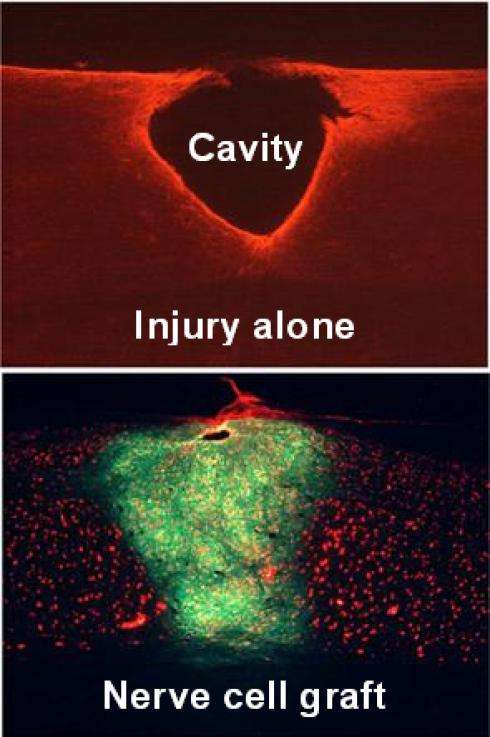 Nerves were not just stimulated in the diaphragm. Ken Kadoya, M.D., Ph.D., of University of California, San Diego, offered details on his work transplanting nerve cells directly into the site of a chronic spinal cord injury (at both two weeks and six months after injury), which then generated new nerves.
Nerves were not just stimulated in the diaphragm. Ken Kadoya, M.D., Ph.D., of University of California, San Diego, offered details on his work transplanting nerve cells directly into the site of a chronic spinal cord injury (at both two weeks and six months after injury), which then generated new nerves.
Kadoya’s team, working in rats, used neural progenitor cells, derived from stem cells, during the transplantation. Over time, these cells matured into new neurons, extending axons for long distances down the spinal cord and connecting with neurons below the injury.
This is an exciting development because the chronic stage of spinal cord injury is “a very refractory state to any current treatments available, because a number of factors inhibit nerve regeneration,” Kadoya said at the press conference.
Kadoya’s particular cells are present in developing tissue and have the added advantage of becoming nerve cells. So, this “nerve replacement approach,” as he called it, is distinct from other currently ongoing stem cell-based trials.
The results showed that six months post-injury, rats that had been inflicted with an injury to the mid-cervical section of the spine showed a cavity, which was then injected with the neuroprogenitor cells. Once injected, the cells “survived, matured and filled the lesion cavity to become many mature neurons,” Kadoya explained.
“When we took a closer look at the whole spinal cord, the grafted nerve cells extended many connections into the whole spinal cord for long distances—from mid-cervical to the thoracic [area of the] spinal cord and made direct connections with host neurons,” he said.
The findings, once further tested, are beneficial and represent another leap towards developing stem cells as a therapy to reverse paralysis after spinal cord injury.

