Does Amyloid Kill in Alzheimer’s, Heal in MS?
 Two groups have recently made strides with amyloid beta (aβ), the supposed main villain in Alzheimer’s disease. But while one group is tackling Alzheimer’s by reducing aβ, the other is tackling multiple sclerosis (MS) by using aβ.
Two groups have recently made strides with amyloid beta (aβ), the supposed main villain in Alzheimer’s disease. But while one group is tackling Alzheimer’s by reducing aβ, the other is tackling multiple sclerosis (MS) by using aβ.
“It’s all fascinating,” Stanford University neurologist Lawrence Steinman told Bioscience Technology. “It is also tough.” For his work indicates amyloid may be both friend and foe--or a friend across the board, an anti-inflammatory that actually alleviates Alzheimer's up front, and may end up doing a lot more for MS in the clinic.
Amyloid as foe
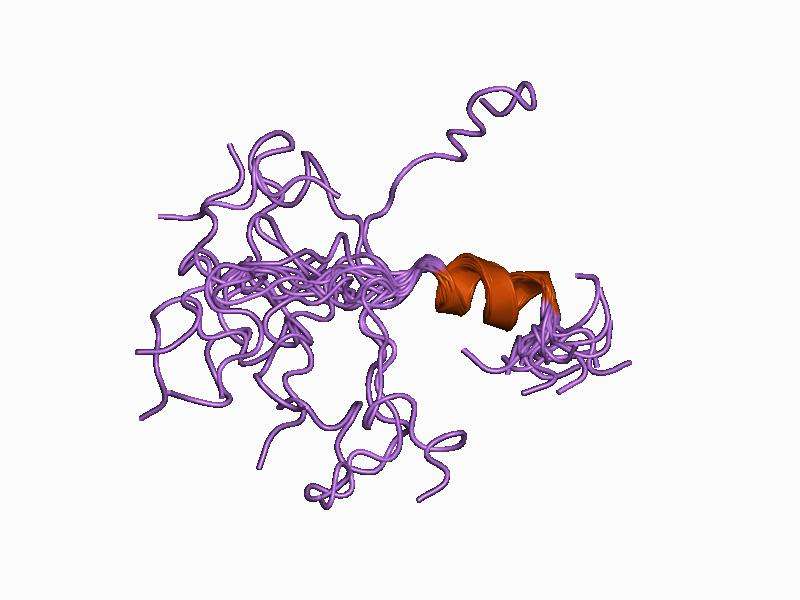
A group led by Lund University biochemist Sara Linse reported in Nature Structural & Molecular Biology this month that a molecular chaperone (helpful protein) named Brichos can nullify many toxic effects of aβ peptide in Alzheimer’s. Past research on mouse brain tissue has revealed that aβ degrades oscillations of the neuronal network in the gamma-frequency band (30 to 80 Hz), important for memory and learning.
But in the recent study, Linse’s team showed this degradation could be completely prevented by Brichos. The team also examined aβ in test tubes with and without Brichos. Brichos was found to bind to aggregated forms of aβ, blocking surfaces that generate neurotoxic activity and cell death.
“I think the paper nicely shows that Brichos is a new player in relation to aβ toxicity, which is conceived as a main pathogenic factor in Alzheimer´s disease,” co-author, and Karolinska Institute neurobiologist, Jan Johannson told Bioscience Technology. “What makes Brichos particularly interesting is that its mechanism is highly specific in reducing toxicity of aβ42, the more aggregation-prone of the two most common variants of aβ produced. These observations, together with the finding that Brichos markedly reduces aβ42 toxicity to the central nervous system (CNS) of Drosophila fruit flies, strongly suggests that targeting Brichos deserves to be investigated as a means to prevent or treat Alzheimer’s disease.”
Johansson said the theory needs testing in animals. “Administering Brichos to mouse models of Alzheimer’s seems like an obvious and necessary next step to validate its effect on pathology and behavioral phenotypes. Getting Brichos over the blood-brain barrier will likely be a challenge, but hopefully less so compared to much larger, glycosylated antibodies, which have been tested in multiple clinical trials. Alternative strategies are increasing the expression, and/or activity, on endogenous Brichos in the human CNS.”
Steinman told Bioscience Technology the Brichos study, in which he was not involved, was “a beautiful piece of chemistry.”
But, he said, a big issue “is whether amyloid is the correct target for modulating Alzheimer’s disease. Is amyloid the big culprit? Should we be chasing amyloid again and again and again?”
Amyloid as friend
Steinman said there has been a dozen or so failed Phase III clinical trials going after mature aβ, or Alzheimer’s in later stages. That stunning run of failures is “leading many to call into question the underlying validity of the amyloid hypothesis,” wrote Massachusetts General Hospital neurologist Bradley Hyman, and Harvard University systems pharmacologist Peter Sorger, in a 2014 Annals of Neurology.
Since those trials went after aβ in later stages, many researchers have switched to focusing on aβ in earlier phases—like the Linse crew.
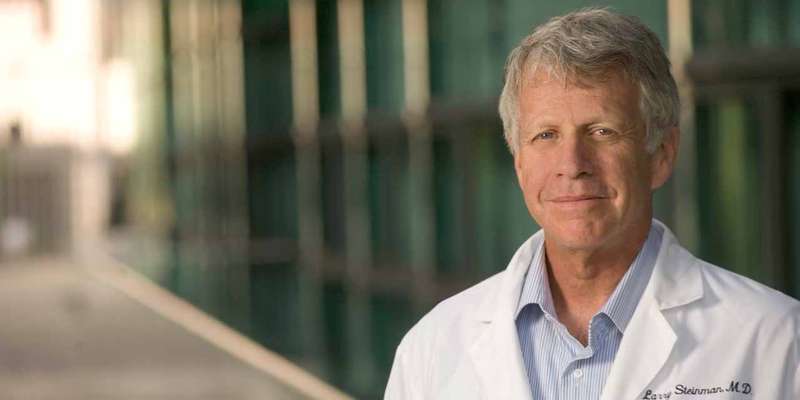 But this has had others—most notably, Steinman’s team—questioning whether aβ is a villain at all. This helped lead Steinman to try an unusual experiment that may pay off in spades—though it may confuse a lot of people along the way. Noticing some aβ in MS lesions, he created a synthetic version of it and gave it systemically to MS-model mice to figure out its purpose there. To his shock, it reversed their paralysis for as long as it was administered. He reported this in Science Translational Medicine in 2012. In 2013, he reported in that same journal that even small, pared down hexa-peptides from aβ—and from other amyloid-forming proteins like Alpha-b crystalline and tau—could reverse paralysis in MS-model mice.
But this has had others—most notably, Steinman’s team—questioning whether aβ is a villain at all. This helped lead Steinman to try an unusual experiment that may pay off in spades—though it may confuse a lot of people along the way. Noticing some aβ in MS lesions, he created a synthetic version of it and gave it systemically to MS-model mice to figure out its purpose there. To his shock, it reversed their paralysis for as long as it was administered. He reported this in Science Translational Medicine in 2012. In 2013, he reported in that same journal that even small, pared down hexa-peptides from aβ—and from other amyloid-forming proteins like Alpha-b crystalline and tau—could reverse paralysis in MS-model mice.
Now “we are tackling neuro-inflammation using amyloid hexa-peptides mostly in models of MS, which is a disease of neuro-inflammation,” he told Bioscience Technology. “In that situation, our amyloid structures definitely make mice better. We have also found the absence of such amyloid structures makes mice worse, whether you knock out aβ or Alpha b-crystallin, or tau, or prion. This could be a whole new potential MS therapy.”
Essentially aβ may act as a kind of molecular chaperone in MS, as Brichos may in Alzheimer’s. The difference is that, where the Brichos chaperone appears to fight the aggregation of amyloid into plaque in Alzheimer’s, aβ appears to fight neuro-inflammation in MS.
It makes sense when considering “there is very little inflammation in Alzheimer’s,” Steinman told Bioscience Technology. The aβ may be fighting it off, as it fights inflammation in MS when injected. Could aβ be a force for some good in Alzheimer’s, keeping neuro-inflammation at bay, while an unknown pathological entity degrades neurons?
Success with MS models
Steinman thinks it is possible. His team has not tested their amyloid hexa-peptides in an Alzheimer’s animal model yet. But they have tried them on MS models so successfully they are already writing the paper. “We are very excited,” he said. There are many drugs for relapsing/remitting MS, but “nothing for progressive MS.” The paper could be published by year’s end. A proof-of-principle trial—perhaps in optical neuritis—could follow. “Things could move really fast then,” he said. And if it is found the hexa-peptides really are “molecular guardians of MS,” the Alzheimer’s field may start viewing amyloid differently.
“There are two big villains in Alzheimer’s, tau protein which forms amyloid, and aβ, which forms amyloid. Amyloid can be good. The pituitary gland stores growth hormones as an amyloid. Beta cells in the pancreas can form amyloid. It can be normal physiology. Amyloid itself may not be bad. A form of amyloid may have pathological characteristics. The idea may end up being to disassemble bad amyloids.”
For MS, his team is not focused on disassembling amyloids, because amyloids—or hexa-peptides isolated from them—have the properties of anti-inflammatories, which is what MS needs. “In the Alzheimer’s brain  there is very little evidence of the kind of classical neuro-inflammation you see in diseases like MS. MS doesn’t look at all like Alzheimer’s. In MS there are T cells, B cells, antibodies, macrophages. In Alzheimer’s you don’t see that.”
there is very little evidence of the kind of classical neuro-inflammation you see in diseases like MS. MS doesn’t look at all like Alzheimer’s. In MS there are T cells, B cells, antibodies, macrophages. In Alzheimer’s you don’t see that.”
Is that because of amyloid? “That’s what I would like to argue. If you take away many of those amyloids- aβ, tau, prions, alpha-B crystallin—you get much worse, classical neuro-inflammation. Too many people talk about Alzheimer’s as an inflammatory disease. It’s not. MS is.”
It is possible the compounds he has tried on MS models—and hopes to try on MS patients—won’t work at all on Alzheimer’s. “Somebody should put it to the test…A model of traumatic brain injury might be relevant,” he said.
But it may be worth trying. There is “considerable evidence that makes people think it is right” that amyloids cause Alzheimer’s, he said. “But so far, clinical trials don’t work.” Brichos and other compounds that interfere earlier in amyloid-formation could be a dead-end, too. “They need to be tried.”
If amyloid isn’t Alzheimer’s culprit, what is? Said Steinman: “We don’t know. But a whole generation of science focused on the idea that amyloid beta is pathogenic, and all phase III trials failed. The last move on the chessboard for the amyloid hypothesis is to intervene really early. That is being tried now. We’ll see.”
Amyloid as anti-inflammatory: “Reproducible and strong”
Meanwhile, his team’s lead compound has given them “a much better understanding of amyloid’s mechanism of action on inflammation. The effect is highly reproducible, and very strong in models of MS and other models of severe inflammation, like stroke.” It has also worked in models of myocardial infarction and optic nerve ischemia, which he will report in the April 1 Journal of Clinical Investigation.
One way or another, Steinman is encouraged.
“I go to the lab every day with a great deal of optimism about this, because the results are so unexpected and fascinating and reproducible. That is all you can hope for.”

