Early in Breast Cancer, Metastatic Cells are Stem Cell-Like, Offering Targets
 Early metastatic breast cancer cells are, strikingly, far more like stem cells than other tumor cells, says a new Nature study. They switch from a dormant (and unnoticed) stem cell-like state in primary tumors, to a more active, virulent state when kick-starting remission years later.
Early metastatic breast cancer cells are, strikingly, far more like stem cells than other tumor cells, says a new Nature study. They switch from a dormant (and unnoticed) stem cell-like state in primary tumors, to a more active, virulent state when kick-starting remission years later.
The discovery could result in earlier detection of—and better drugs for—metastatic breast cancers.
“This paper is an important addition to an area of research of high biological and clinical relevance, but woefully understudied to date,” Memorial Sloan Kettering Cancer Center Director Joan Massagué, Ph.D., told Bioscience Technology. Massagué was uninvolved in the study. “Much work on metastasis over the past decade has centered on processes that let cancer cells in primary tumors invade and move into the circulation for metastatic dissemination. Unfortunately, when a tumor is diagnosed, these processes have been ongoing for months, if not years, and clinically don't matter much. The horses are out of the barn. What matters from that point is not so much how cancer cells disperse from the tumor, since the primary tumor will be removed by a surgeon immediately in most cases. What matters at that point are the properties and vulnerabilities of already disseminated cells that constitute the seeds for future metastatic outgrowth.”
Said Massagué : “What is the nature of these cells? In what organs and tissues do they reside? What protects them from immune system elimination? What sets them off to grow? Do they succeed every time they attempt to grow? What drugs could kill them when they attempt to grow? Better, what drugs could kill them when they are dormant? The Nature paper addresses the first of these questions, and provides further evidence metastasis is seeded by cancer stem cells. The insight is not entirely surprising, but it is welcome.”
Read More: Women With MRI Abnormality Nine Times More Likely to Get Breast Cancer
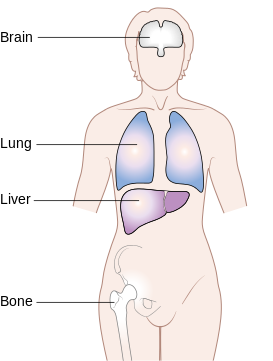
Jenny Chang, M.D., director of the Houston Methodist Cancer Center, told Bioscience Technology: “Overall, this is a great paper. Its authors must be applauded for their ability to collect these cells from mice bearing human cancers. The novelty is in the capture of these cells. Since the mice are growing human cancers, the isolation of any human cell must by definition be metastatic. Interesting but not surprisingly, these `human’ metastatic cells harbored many `stem cell’ markers. Consistent with some earlier studies that metastatic cells in different organs might be distinct, the authors found that brain metastases were very different and most stem-like.” Chang was also uninvolved in the study.
 Agreed University of Utah Huntsman Cancer Institute associate professor Alana Welm, Ph.D.: “These data are very exciting. They reveal the heterogeneity of metastatic breast cancer cells at the single cell level, using state-of-the-art models of human breast cancer.” Welm, also uninvolved in the study, told Bioscience Technology: “Even more importantly, these data uncover key differences between metastatic cells that appear to be in a dormant state versus those in an actively growing state.”
Agreed University of Utah Huntsman Cancer Institute associate professor Alana Welm, Ph.D.: “These data are very exciting. They reveal the heterogeneity of metastatic breast cancer cells at the single cell level, using state-of-the-art models of human breast cancer.” Welm, also uninvolved in the study, told Bioscience Technology: “Even more importantly, these data uncover key differences between metastatic cells that appear to be in a dormant state versus those in an actively growing state.”
One rogue cell
One reason all early cancers are dangerous is that all it takes is one rogue cell, breaking off a primary tumor, to restart cancer post-surgery. Such cells can drift through the blood, hide in a tissue, and lie dormant for years.
But the nature of those rogue cells has remained elusive. What qualities do they possess to survive long periods in the hostile environments of new organs? Many have speculated they must be stem cells, which are more potent than average cells. But despite lack of data, only seven percent of breast cancer funds have been dedicated to the search for the rogue cells.
A group led by oncologist Zena Werb of the University of California San Francisco (UCSF) set out to find them. Earlier, Werb and others identified groups of cells at breast tumor margins that seemed on the verge of metastasis. The thought was the cells’ proximity to the bloodstream—and to nurturing proteins in the tumor microenvironment—switched on stem-cell genes. Breast stem cells are multipotent cells that form breasts in puberty, and prompt breast growth in lactation.
For the new project, Werb’s team used the patient- derived xenograft (PDX) technique. First, they transplanted human tumor cells into mice. These mutated human metastatic cells stood out from the healthy mouse cells. Then they used a flow cytometry technique, which they devised, to trap single human metastatic cancer cells traveling in mouse blood, or landing elsewhere. Finally, they used newly-developed microfluidic technology to analyze the elusive cells’ expressed genes.
The elusive stem cell mets
When Werb’s team looked at patterns of gene expression in human cancer cells retrieved from different tissues of the PDX mice, they discovered major differences between early and later-stage metastatic colonies. In metastases throughout organs, the cancer cells' gene activity looked similar to that of the original primary tumors transplanted into the mice (if they possessed some minor features mirroring those of their new host organs).
Meanwhile, early-stage metastatic cells, and cancer cells escaping primary tumors in blood, expressed genes active in breast stem cells—very different from primary tumor cells. These cells expressed genes associated with dormant, undifferentiated states linked to cell death immunity. This, the team guessed, is what may let metastatic cells survive in new environments.
Identical gene expression patterns were seen in metastatic cells in mice whose tumors came from genetically and clinically diverse human patients. Metastatic gene programs clearly were not dependent on primary tumor genetics.
Drug supports theory
Since mets starting to mature, or differentiate, into secondary tumors expressed high levels of the genes cMYC and CDK2, the team gave 24 PDX mice dinaciclib, a CDK inhibitor that kills off cells expressing high levels of MYC. While 44 percent of control mice (11 of 25) “relapsed”—developed secondary cancers— in four weeks, the team could only see metastatic cells in one drug-treated mouse: a mere four percent.
The drug nearly wiped out the metastases, leaving the primary tumor intact.
The study’s single-cell techniques are being used by a consortium of UCSF researchers to tackle many biological and clinical questions.
Two novel findings
“There are two major 'firsts' in this study,” lead author Devon Lawson, PhD, told Bioscience Technology. A UCSF post-doc during the study, she is now a University of California Irvine assistant professor of physiology and biophysics. “The first is technical. We developed a highly sensitive and specific flow cytometry-based assay which let us isolate metastatic cells in engrafted mice, based on species differences between the host (mouse) and graft (human). This assay was key. It enabled us to isolate rare metastatic cells at very early stages of the metastatic process, when there were only a few cells observed in the periphery—which we called ‘low-burden.’”
Said Lawson : “The second 'first': we found these low-burden metastatic cells have a distinct signature, and were more like the basal/stem cells from the normal mammary gland we profiled. Higher burden metastatic cells were more luminal-like [differentiated]. Although diversity in cancer cell phenotypes has been well documented at the genetic and phenotypic level, these distinct differences correlating with burden are novel, and imply that metastatic cells have different phenotypes and functions as they seed and grow.”
The group did not “directly” study longevity-associated qualities of cancer stem cells. But “we indeed found the low-burden metastatic cells [in primary tumors] had a less proliferative signature. We also found they expressed higher levels of anti-apoptosis genes, like bcl2 and bcl2l1. This may represent a protective mechanism. We believe the 'stem-like' nature of these cells, when they first metastasize, probably helps them seed and survive in a foreign microenvironment, as they may be more plastic and, therefore, adaptable. Also, this stem-like program may be necessary for them to produce a new metastatic tumor.”
CDK inhibitors may target healthy stem cells, in addition to cancer stem cells. Lawson told Bioscience Technology: “The CDK experiments in our study were meant more as proof-of-principle than as a real therapeutic avenue. CDK inhibitors are in clinical trials for many cancers, although not specifically indicated to treat metastasis. CDK inhibitors are showing side-effects in humans, and likewise some of the mice in our study developed weight loss and skin lesions. Since they inhibit cell cycle, it makes sense they have many side-effects. They may spare normal and cancer stem cells if they are not proliferating, but we did not directly test this.”
Caveats
Welm said the study is clinically very promising. “Understanding critical `switches’ that must occur for micro-metastatic cancer cells to convert to overt metastatic lesions— such as activation of the MYC-CDK2 axis—offers opportunities for therapeutic approaches to keep cancer in the dormant state,” she told Bioscience Technology. “Similar therapies might even work to arrest or eliminate established metastases, which could finally lead to an effective treatment regimen based specifically on the unique biology of metastasis.”
However, she said, PDX models “are not perfect representations of human breast cancer. A major caveat of PDX models is the lack of a functional immune system, as well as lack of many other tumor-host interactions. In PDX models, the human tumor is growing in a mouse host, and some mouse host proteins and hormones do not fully activate their counterpart human receptors. Since the immune system and other host factors are almost certainly involved as determinants of whether micro-metastases grow into overt lesions, research using such models has to be interpreted with caution.”
Agreed Chang: “One caveat, remember that these mice are immunocompromised, and the complex interplay between cancer, metastases and immunity cannot be delineated by this study.”
On the other hand, Welm said, such models “offer a unique opportunity to examine micro-metastatic cancer cells living within organs usually not accessible for research in patients.”
Another question may be “how conserved the determinants of metastasis are between different breast cancer subtypes and individual patients. For feasibility reasons, the present study only examines PDX models from three patients with triple negative breast cancer. It remains to be seen whether the heterogeneity of metastatic determinants will be consistent enough across patient groups to facilitate development, and testing of new therapies with traditional clinical trial designs, or whether a more personalized approach will be required.”
Importantly however, Massagué concluded: “The methods for cell isolation and single cell analysis the authors employed should be useful for more studies of this kind, and encourage more research on this important problem.”





