The First Personalized Genomic Cancer Vaccines
 The first personalized cancer vaccine using genomics to define targets elicits robust immune responses, says a recent Science study. After running an exome analysis of three melanoma patients’ tumors, a team led by Washington University researchers chose seven tumor missense mutations from each patient most likely to elicit immune responses—and made personal vaccines.
The first personalized cancer vaccine using genomics to define targets elicits robust immune responses, says a recent Science study. After running an exome analysis of three melanoma patients’ tumors, a team led by Washington University researchers chose seven tumor missense mutations from each patient most likely to elicit immune responses—and made personal vaccines.
Each patient was found to have existing T cells to one of the mutations, numbers further boosted by the vaccines. And in each patient, impressive armies of new T cells appeared that specifically targeted tumor neoantigens created by two of the other seven mutations.
“This is very promising," leading cancer immunotherapy researcher Carl June M.D., told Bioscience Technology. June, with the University of Pennsylvania, was not involved in the current study. "This is the first demonstration in cancer patients that neoantigens created by missense mutations can serve to generate high frequency responses in cancer patients after therapeutic vaccination."
"This paper is really interesting because of the completeness of its analysis of tumors of three patients," pioneering cancer immunologist Thierry Boon told Bioscience Technology. Boon, former chief of the Ludwig Institute for Cancer Research Brussels branch, was also uninvolved in the current study.
Genomics approaches
Other researchers—most notably Stephen Rosenberg of the National Cancer Institute (NCI)— have long noticed that robust immune responses can be generated when patient T cells are intensely co-cultured with bits of their tumors. However, despite some spectacular tumor regressions, the newly generated T cells did not last long, often only days. Improvements helped. Depleting the body of T cells before infusions can result in a massive expansion of targeted T cell infusions once in vivo, to the point where they can comprise 80 percent of CD8 T cells months later, according to a review by Rosenberg and the NCI’s Nicholas Restifo in the same issue of Science.
Another improvement has been ensuring that less differentiated, more stem-cell like T cells are created and infused, as these cells can live in the body for over a decade.
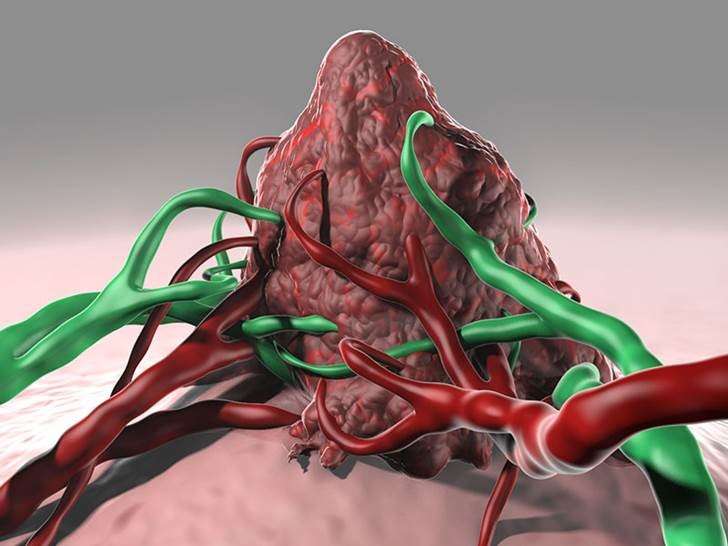
However, recently, Rosenberg’s group and others have been working on an approach that may significantly increase the number of relevant targets pursued, critical as tumors are proving so heterogeneous. Cheaper deep sequencing techniques have let them generate many T cells, exquisitely targeted to peptides produced by many unique tumor gene mutations, at once. They have achieved this in different ways, including comparing tumor exomes (protein-encoding DNA) with normal exomes in patients; calculating which peptides may bind tightly to key T cells; generating peptides from those mutated genes; coculturing the resulting peptides with patient T cells to alert and alarm the T cells to (and by) the presence of the mutated tumor peptides—and infusing the newly educated T cells back into patients.
Rosenberg has said he believes personalized cancer immunotherapies may prove seminal, given the heterogeneity of many cancers.
Read More: An Introduction To Immunotherapy And The Promise Of Tissue Phenomics
The new vaccine approach
The Washington University group has accomplished a similar feat, but in a vaccine, and with twists. They generated tumor (protein-encoding) exomes. They generated RNA from those. This winnowed out the approximately 50 percent of mutated genes that were not expressed; not actively producing mutated proteins/peptides. They tested to determine which of these neoantigens appeared on the outside of tumor cells—so were easily targetable by T cells. They ran an algorithm to identify which neoantigens might prompt robust immune responses due to their differing abilities—predicted by analyzing structure—to bind to T cells.
Seven remaining antigens were fed to patients’ dendritic cells (DCs), which are antigen presenting cells. The DCs were then infused, to act as vaccines, into patients three times in four months.
The DC vaccines prompted a robust proliferation of T cells specific to three of the seven chosen antigens in each patient—and surprisingly, to other cancer antigens. All three patients remained stable for several months, although they had also taken other drugs, so outcome causes can’t be known. The study was not designed to measure clinical effectiveness. It was designed to see if highly variegated precision T cell armies can be raised to tumors by a vaccine. They can.
Many firsts
Among firsts scored by this vaccine: it was the first “to use genomics up front to define the neoantigens that are highly specific to each patient, then test them with patient-derived material before the vaccine peptides are defined,” co-author Elaine Mardis Ph.D., told Bioscience Technology. Mardis is co-director of the Genome Institute of Washington University.
 “We used conventional in vitro lab assays, called ‘Elispot,’ with an isolate from each patient, to refine the list of peptides we generated from the work above (genomics, comparison of binding affinity),” Mardis said. “The Elispot assays serve as a patient-specific check on the algorithm's predictions. From this list of peptides, the top seven were chosen for GMP manufacturing, and the cocktail of peptides were co-cultured with dendritic cells isolated from the patient to make the vaccine….Once the patient received the vaccine doses, we monitored by flow cytometry to evaluate whether the production of peptide-specific T cells was being stimulated.”
“We used conventional in vitro lab assays, called ‘Elispot,’ with an isolate from each patient, to refine the list of peptides we generated from the work above (genomics, comparison of binding affinity),” Mardis said. “The Elispot assays serve as a patient-specific check on the algorithm's predictions. From this list of peptides, the top seven were chosen for GMP manufacturing, and the cocktail of peptides were co-cultured with dendritic cells isolated from the patient to make the vaccine….Once the patient received the vaccine doses, we monitored by flow cytometry to evaluate whether the production of peptide-specific T cells was being stimulated.”
The approach so far promises to effectively address tumor heterogeneity.
“Our approach does consider heterogeneity by evaluating, using genomics, the common neoantigens present in several metastatic lesions,” Mardis told Bioscience Technology. “Therefore, we develop the most broadly tumor-reactive set of T-cells. What we hope is that, like many other types of immunotherapy, we can establish that patients will have lasting or ‘durable’ responses, and they may indeed need only a single course of treatment.”
The durability of the response is not optimal right now. “The peak response occurred eight weeks after the last vaccine round, and one of the open questions about this approach is whether patients will continue to have a durable response,” Mardis said. “It's simply too early to know [although] we do think we can potentially culture the activated T cells so that patients can have a 'booster shot' if needed.”
Mardis can “absolutely” imagine bolstering the vaccine with complimentary therapies. “We do anticipate a second trial that combines the precision vaccine with a checkpoint blockade therapy to evaluate whether this is a better ‘tweak’,” she said.
Issues
June has some reservations. “The main scientific issue facing the field is whether there will be escape by the tumors after vaccination with passenger mutant peptides,” he told Bioscience Technology. “The main engineering issue is how long it will take to develop technology to scale out this highly personalized technology for widespread availability.”
Overall, he said, “I think the major issue is what will be the frequency of escapes, since most of the targets are not driver mutations.”
In response, Mardis noted that, “in Figure 1A of the manuscript, we demonstrate that by sampling from several different tumor isolates for two of the patients, we were able to identify shared tumor-unique neoantigens. This is our current approach and is aimed at identifying neoantigens that make the vaccine most broadly of therapeutic benefit, in principle. “
Additionally, Mardis said, the digital nature of massively parallel sequencing data “enables us to also select the neoantigen candidates that are present in the founder clone of the tumor. We know from several studies of cancer progression that, while subclones may come and go in tumor evolution, the founder clone persists. Hence, the strategy we are pursuing to focus on founder clone neoantigens should help against the escape phenomenon that Dr. June has raised. “
But the bottom line, said Mardis, is that “Dr. June's comments are important considerations, and it is simply too early to know what course the disease will take after dendritic cell vaccination. Since these are early studies, we simply have more unanswered questions than answers.”
Establish your company as a technology leader. For 50 years, the R&D; 100 Awards, widely recognized as the “Oscars of Invention,” have showcased products of technological significance. Learn more.

